What Is a Disc Herniation? Why Language Matters in Your Recovery
Back pain is one of the most common complaints people seek help for, and one of the most misunderstood. If you’ve ever been told you’ve “slipped a disc,” you’re not alone — but you’ve also been given a phrase that’s not accurate and often unhelpful. At Movement — Health & Wellness, we take a different approach. We explain clearly what’s happening inside your body and avoid language that can make your pain feel scarier than it is.
What Actually Is a Disc Herniation?
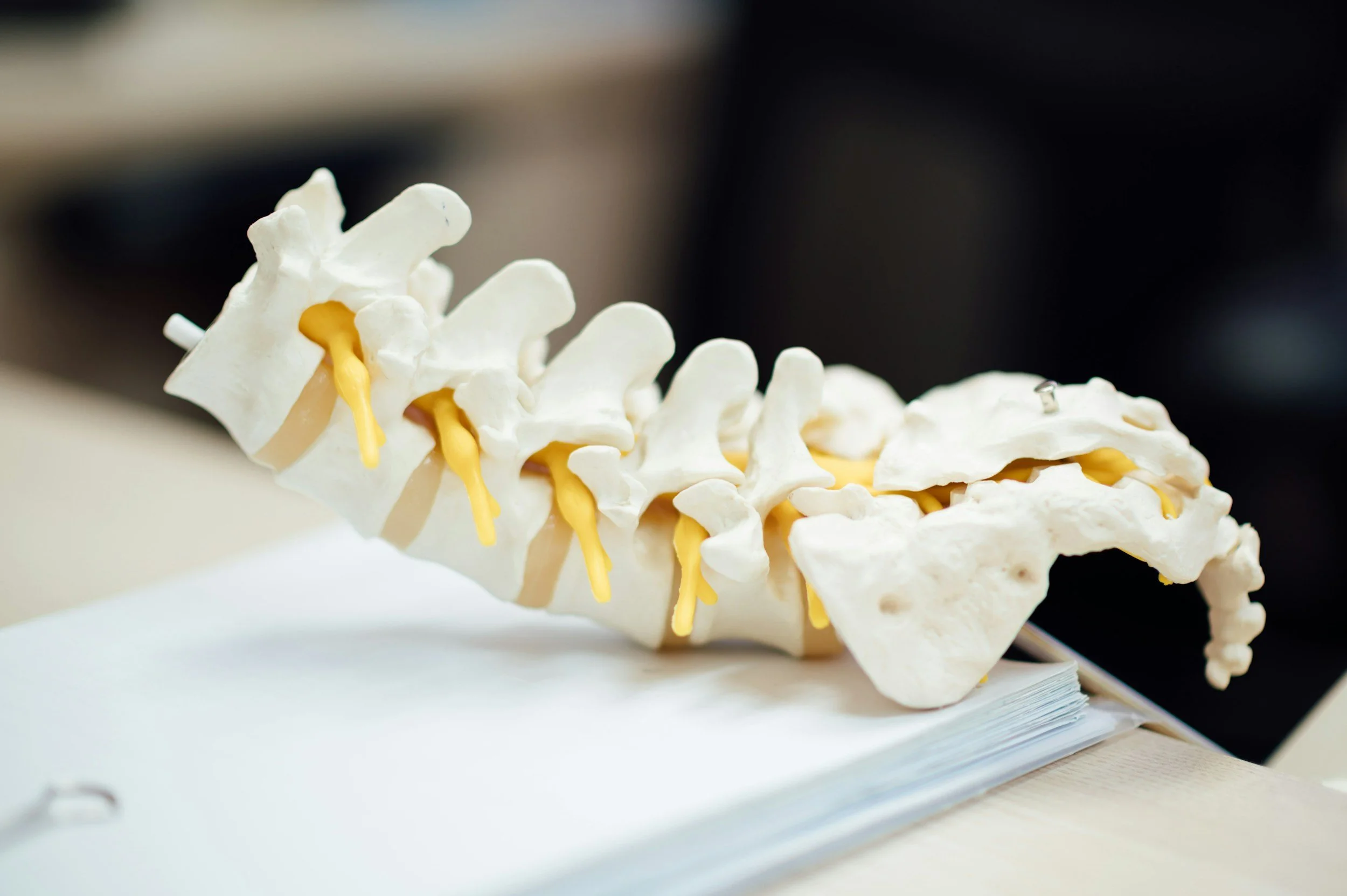
Between each bone in your spine sits a disc — a tough, fibrous outer layer (the annulus fibrosus) with a softer, gel-like centre (the nucleus pulposus). These discs act like shock absorbers and help your spine move smoothly.
A disc herniation happens when some of the inner material pushes through small cracks in the outer layer. This can irritate or compress nearby nerves and cause pain, tingling, or weakness in the area those nerves supply.
Here’s what’s important to understand:
The disc does not “slip” out of place.
The bones of your spine remain structurally stable.
Disc changes are often part of normal ageing, and many people have herniations with no symptoms at all.
Clear terminology helps you make sense of your body — and reduces fear.
Why I Don’t Tell Patients They’ve “Slipped a Disc”
The phrase “slipped disc” is outdated and misleading.
It gives the impression that the disc has popped out of the spine or that something is dangerously unstable — neither of which is true.
Using phrases like “slipped,” “crushed,” or “worn out” has been shown to:
Increase fear and anxiety
Make people believe their spine is damaged or fragile
Lead to movement avoidance
Slow down recovery
Create long-term negative beliefs about the back
In reality, the spine is incredibly strong, adaptable, and capable of healing. Disc herniations often improve with time, load management, movement, and the right therapeutic plan.
What the Science Says About Disc Herniations
Most disc herniations improve without surgery
High-quality research shows that many herniations shrink or reabsorb over time as inflammation settles. Pain typically improves over weeks to months.
2. Surgery can help some people — but long-term outcomes are often similar
Randomised controlled trials demonstrate that while surgery may speed up early relief (especially for severe leg pain), conservative care often leads to similar results at 6–12 months.
3. The type of herniation matters
Extrusions and sequestrations (where more material has moved out of the disc) are actually more likely to regress naturally than small bulges. This surprises many people.
Why Language Shapes Your Recovery
Something we don’t speak about enough in healthcare is how much the words you hear influence:
your pain
your function
your beliefs
and your prognosis
Research on nocebo effects (the opposite of placebo) shows that negative or alarming language from clinicians can increase pain, disability, and fear of movement.
For example:
“Your spine is degenerating”
“Your disc is crushed”
“Avoid bending or you’ll make it worse”
These messages create fear and physical guarding — and this delays recovery.
At Movement — Health & Wellness, you’ll get clear, calm, evidence-based explanations that empower you, not frighten you.
What This Means for You
If you’ve been diagnosed with a disc herniation:
You are not broken.
Your disc has not slipped out of place.
You can still move, strengthen, and participate in the activities you love.
Most disc injuries improve with the right plan and guidance.
You’ll receive a tailored approach that includes hands-on care (if needed), a progressive exercise plan, reassurance, and movement strategies so you feel confident again.
Want to learn more about ways we can help you?
Schedule a free discovery call today or make an appointment
References
Peul WC et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007.
Bailey CS et al. Surgery versus conservative care for persistent sciatica. N Engl J Med. 2020.
Jacobs WCH et al. Surgery vs conservative management of lumbar disc herniation: systematic review. Spine. 2011.
Chiu CC et al. Probability of spontaneous regression of lumbar disc herniation: systematic review. 2015.
Kesikburun B et al. Spontaneous regression of extruded lumbar disc herniation. PLoS One. 2019.
Rashed S et al. Predictive factors for resorption of lumbar disc herniation: meta-analysis. J Neurosurg Spine. 2023.
Blasini M et al. Nocebo and pain: psychoneurobiological mechanisms. Neurosci Biobehav Rev. 2017.
Daniali SS, Flaten MA. Effects of provider characteristics on placebo/nocebo and pain outcomes: systematic review. Front Psychiatry. 2019.
Fardon DF et al. Lumbar disc nomenclature 2.0. Spine J. 2014.